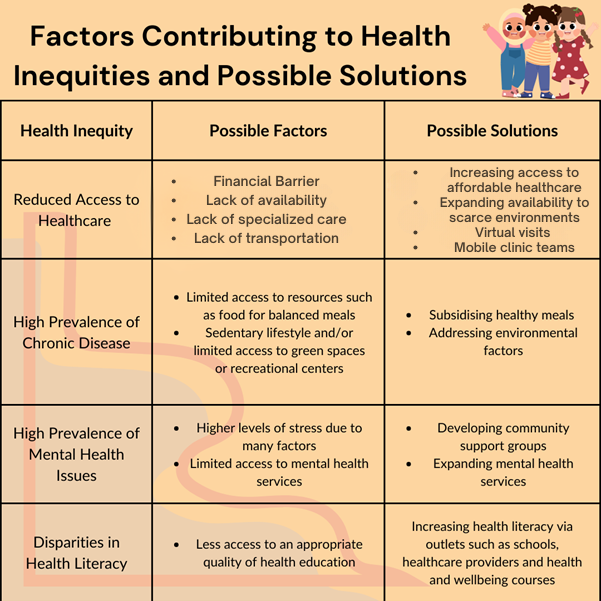
Health inequities remain a serious issue in healthcare, especially for newborns at risk for brain conditions, where early help can make a big difference in their lives. Social determinants of health are social and economic conditions that affect many health outcomes. These issues are important for children with conditions that harm early brain development, like neonatal stroke, premature birth, or congenital heart disease. Challenges like financial hardships, belonging to certain racial or ethnic groups, and lower parental education are linked to poorer developmental outcomes for preschool-aged children born very early or with low birth weight. These examples show that medical problems and social difficulties are connected, stressing the need for early support.
Services like speech and occupational therapy can help address delays caused by early hardships. However, many families are unable to access these services within three months of leaving the NICU. This drop-off is often attributed to difficulties accessing ongoing care, especially for disadvantaged families. Studies show that social factors affect healthcare use. For instance, preterm babies born to mothers who do not speak English or who live in poor neighborhoods are less likely to get follow-up care. These challenges show how social and structural barriers can prevent families from accessing the care they need, creating health inequities from birth.
Perinatal arterial ischemic stroke (AIS) is a type of stroke that can happen to babies. AIS happens when a blood vessel in the brain is blocked, affecting more than 100,000 children in North America. While the risk of death from AIS is relatively low, it often causes long-term problems. These include motor difficulties, delayed language, learning problems, epilepsy, behavioral challenges, and vision issues. But it is not just about the stroke itself. Health inequities can change how babies get treated after a stroke. These inequities can affect how fast and how well they receive care and support. These outcomes show why early treatment and consistent care are vital as children grow into teens and adults.
Despite the importance of specialized care, little research explores the impact of race, income, or other social determinants on accessing services or outcomes for AIS. Specifically, it is important to understand factors influencing follow-up care or long-term support for these children. This gap means that future studies will need to focus on how social challenges affect care for babies with neonatal AIS. On the bright side, researchers from Toronto, Canada recently explored this topic and presented preliminary data at the International Child Neurology Congress 2024 in Cape Town, South Africa. The study examined how poverty and neighborhood diversity affected healthcare use and neurological outcomes in babies with neonatal AIS. Understanding these connections can help improve care, make healthcare more equal, and reduce lifelong disabilities in children worldwide.
Strategies for Practitioners to Close the Gap and Promote Equitable Health:
Screen for Social Determinants of Health (SDOH)
- Use validated screening tools to identify families facing challenges such as poverty, housing instability, food insecurity, or language barriers
- Integrate SDOH assessments into routine care and ensure they are revisited at follow-up appointments
Build Multidisciplinary Teams
- Collaborate with social workers, case managers, and community health workers to provide families with tailored support
- Engage cultural liaisons or interpreters to bridge language and cultural gaps
Partner with Community Resources
- Connect families to local organizations offering financial assistance, housing support, early childhood education, or therapy services
- Work with non-profits or government programs to ensure long-term developmental support
Implement Health Equity Practices
- Train providers and staff on implicit bias and cultural competence to ensure equitable treatment for all families
- Routinely evaluate healthcare practices and outcomes by race/ethnicity, socioeconomic status, and other SDOH to identify disparities
- Social Determinants of Health – Healthy People 2030 | health.gov. https://health.gov/healthypeople/objectives-and-data/social-determinants-health (2020).
- Chabrier, S. et al. Multimodal Outcome at 7 Years of Age after Neonatal Arterial Ischemic Stroke. The Journal of Pediatrics 172, 156-161.e3 (2016).
- Wagenaar, N. et al. Neurodevelopment After Perinatal Arterial Ischemic Stroke. Pediatrics 142, e20174164 (2018).
- Felling, R. J. et al. Predicting Recovery and Outcome after Pediatric Stroke: Results from the International Pediatric Stroke Study. Ann Neurol 87, 840–852 (2020).
- Lee, J. et al. Maternal and Infant Characteristics Associated With Perinatal Arterial Stroke in the Infant. JAMA 293, 723–729 (2005).
- deVeber, G. A. et al. Epidemiology and Outcomes of Arterial Ischemic Stroke in Children: The Canadian Pediatric Ischemic Stroke Registry. Pediatr Neurol 69, 58–70 (2017).
- Linsell, L., Malouf, R., Morris, J., Kurinczuk, J. J. & Marlow, N. Prognostic Factors for Poor Cognitive Development in Children Born Very Preterm or With Very Low Birth Weight: A Systematic Review. JAMA Pediatrics 169, 1162–1172 (2015).
- Parker, M. G. et al. Associations of household unmet basic needs and health outcomes among very low birth weight children. J Perinatol 43, 364–370 (2023).
- Agrawal, N., Johnston, S. C., Wu, Y. W., Sidney, S. & Fullerton, H. J. Imaging Data Reveal a Higher Pediatric Stroke Incidence Than Prior US Estimates. Stroke 40, 3415–3421 (2009).
- Spicer, A. et al. Health Status and Health Service Utilization of Infants and Mothers During the First Year After Neonatal Intensive Care. Advances in Neonatal Care 8, 33 (2008).
- Fraiman, Y. S., Stewart, J. E. & Litt, J. S. Race, language, and neighborhood predict high-risk preterm Infant Follow Up Program participation. J Perinatol 42, 217–222 (2022).
About the Author

Esha Parakh

Akshat Pai
Graphics: Akshat Pai and Esha Parakh
Medical Editors: Mesha Martinez, MD
Junior Editor: Neha Suresh Ramiah