Introduction – Why I Chose This Topic
Introduction – Why I Chose This Topic
Hi! My name is Christina Rothfuss, and I am studying occupational therapy (OT) at Southern California University of Health Sciences. In school, I learned that it is important to be ready to help people with many different health problems. I became interested in pediatric stroke because, like a lot of people, I did not know that strokes could happen in babies and kids. After learning how much occupational therapy can help these children, I wanted to find out how well students are taught to work with them.
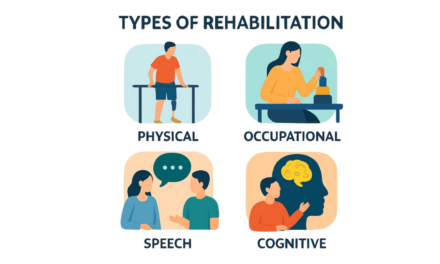
What is Occupational Therapy?
OT helps people of all ages do everyday activities or “occupations” by addressing physical, cognitive, sensory, and emotional challenges. While physical therapy (PT) focuses on improving movement and strength, OT typically supports independence by adapting tasks, teaching new skills, and modifying environments.
For children who’ve had a stroke, OTs help improve movement, coordination, and daily skills like play, learning, and self-care. They support thinking, sensory, and emotional development by using strategies that tap into the brain’s ability to form new connections. Since a child’s brain is still growing, therapy in children can have especially powerful neuroplastic effects. Neuroplasticity—the brain’s way of making new connections and relearning skills. OTs use strategies that support neuroplasticity to help children grow and take part in everyday activities that promote their health and development.

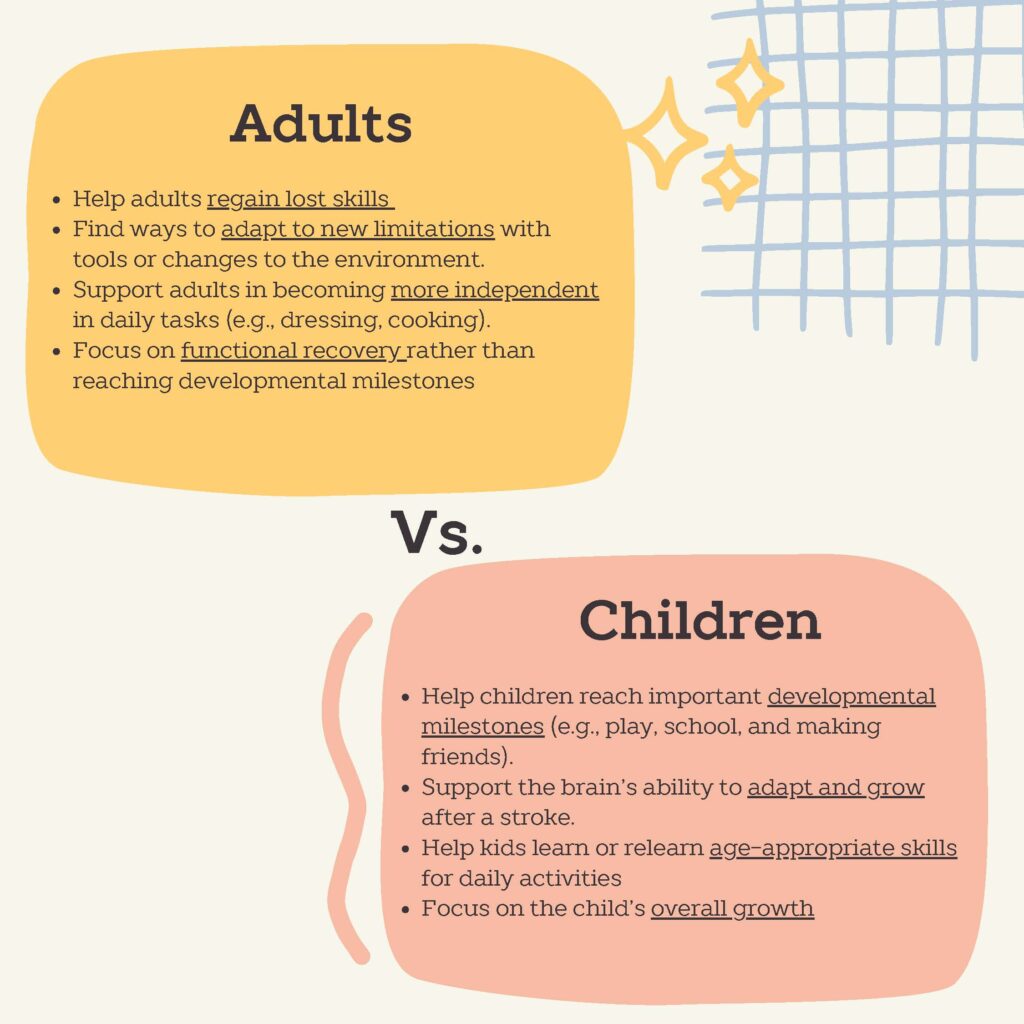
Why Age Matters
Age plays a crucial role in stroke recovery, as children and adults have different developmental needs and healing abilities. Because of these differences, treatment techniques and therapy goals must be tailored accordingly. As children grow and activity demands increase with age, they may develop new challenges. This is why early intervention and consistent support are key parts of therapy. That being said, keeping follow-up appointments, even when progress looks good, is important to help the child continue to adapt and thrive.
Current State of OT Education
Learning about how OTs help children after a stroke made me curious about how well students are trained to work with these kids. To find out, I researched how OT programs teach pediatric stroke and spoke with therapists who specialize in this area. Through my research and conversations with professionals, I gained a deeper understanding into the complexities and challenges OT programs face in preparing students for lesser-known conditions.
From My Research:
Most stroke research is about adults, however more studies are looking at kids, especially those with one-sided weakness from perinatal stroke, called unilateral cerebral palsy (CP). Two strong therapy approaches are Constraint Induced Movement Therapy (CIMT), which helps the weaker arm by limiting the stronger one, and Bimanual Therapy (BMT), which builds two-handed skills. Research shows both are equally effective, which is helpful since CIMT can be costly and isn’t always the best fit for every child. Also, despite the growing evidence supporting CIMT, many therapists lack training or clear guidelines, which can affect their confidence and willingness to use it in practice.
From Talking with Therapists:
Lifelong learning is essential for effective therapy practice. While school provides a general foundation, 82% of therapists in a recent survey said they learned to treat pediatric stroke primarily through mentorship, and real-life experience. This shows the importance of being ready to grow beyond the classroom and to stay current with best practices and new diagnoses.
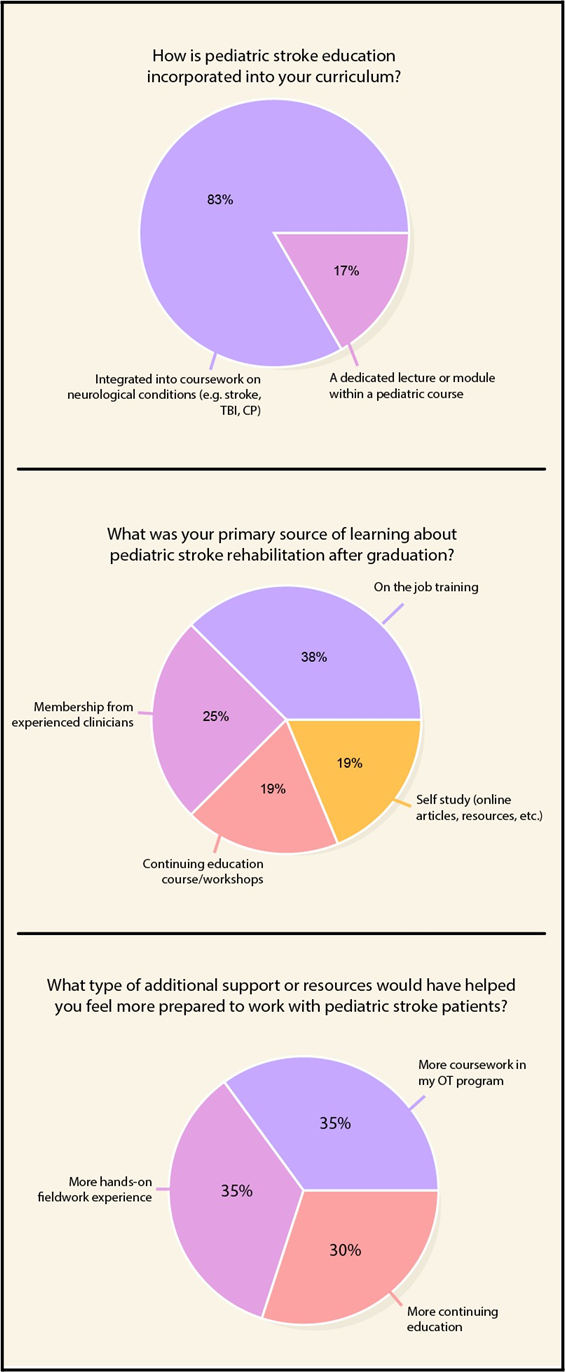
From My Survey:
Although pediatric stroke is a leading cause of unilateral CP, educational programs tend to emphasize CP more broadly, with only 1 to 3 hours dedicated specifically to pediatric stroke as an underlying cause. Encouragingly, many OT programs and therapists express a desire for more hands-on training and education to strengthen their clinical skills and better support children affected by stroke.
Looking Ahead: How We Can Enhance OT Education
There is a strong need for more pediatric-specific education, hands-on training, and resources to help support OTs in feeling better prepared and confident when working with pediatric stroke populations. While schools can’t cover every possible diagnosis, it’s important to emphasize teaching adaptability, resourcefulness, and how to handle new challenges. Incorporating specific case studies, practice activities, and real-world experience with proven methods like (CIMT) and (BMT) can greatly improve therapist skills and confidence. Emphasizing that strokes can occur at any age and teaching how to support children and families facing sudden disabilities would strengthen training, and ultimately lead to better care and outcomes for children and their families.
For Parents: What to Look for in an OT Facility
Not every OT clinic is the same, especially when it comes to treating children who have had a stroke. As a parent, it is important to know what to look for when picking a clinic. Here are some key things to keep in mind:
- Finding the Right Fit
When choosing a therapist consider asking them about their approach to therapy. A strengths-based empowering OT, regardless of specific stroke experience, can make a big difference in helping your child grow in confidence and ability.
- Understanding your Treatment Options
Don’t hesitate to ask your therapist about the research behind their treatment approach. Pediatric stroke shares many features with unilateral CP, and a knowledgeable OT can draw from this research to explain evidence-based strategies that are tailored to your child’s unique needs, strengths, and preferences.
- Whole-Child Focus
Choose a clinic that looks at all parts of your child’s growth, including movement, thinking, social skills, sensory needs, emotional health, and daily activities at home, school, and in the community. A good OT will check your child’s strengths and needs, then set clear goals that match your family’s priorities. Full recovery may not always be possible, but therapy works to reduce the stroke’s effects and help your child live a happy, active life.
- Family Involvement
Pick a clinic that includes parents in the therapy process. When parents are part of the plan and know how to help at home, it is easier for the child to keep improving outside of therapy sessions.
- Ongoing Learning
Ask how the therapists stay updated with the newest research about pediatric stroke. Also, find out if they receive ongoing training, support, or advice from experts.
For Therapists: Approaching Less Familiar Diagnosis with Confidence
One effective way to empower both students and practicing therapists is to shift from diagnosis-focused thinking to a function focused approach. By examining how a condition impacts a child’s movement, function, and participation, OTs can apply current research from similar conditions, like unilateral cerebral palsy, to make the most of the available evidence. Additionally, having easy access to these resources within the workplace can help therapists make informed, evidence-based decisions with greater confidence, especially when working with less familiar diagnoses. Below is a list of resources therapists can use to help support their knowledge and clinical skills, and parents too.
Resources:
Parents and Caregivers
Levy, T. J., & Hoare, B. (2023). Therapy choices for children with difficulties using 1 hand after a brain injury. Archives of Physical Medicine and Rehabilitation, 104(8), 1363–1366. https://doi.org/10.1016/j.apmr.2023.02.026 https://iapediatricstroke.org/wp-content/uploads/2024/03/TherapyChoicesForChildrenWithDifficultiesUsing1Hand_2023.pdf
Alliance, C.P. Identifying the right intervention for your child. https://cerebralpalsy.org.au/wp-content/uploads/2023/06/GuidetoCPInterventionsPDF_.pdf
Parents guides for early assessment/diagnosis, early intervention therapy 0-2, early intervention therapy preschoolers, therapy and support for school-age children.https://cerebralpalsy.org.au/cerebral-palsy/treatments/
Websites and Continuing Education
https://iapediatricstroke.org/research-findings/
https://www.physio-pedia.com/Physiotherapy_Treatment_Approaches_for_Individuals_with_Cerebral_Palsy
References:
Guidelines and Systematic Reviews
Hoare, Brian J et al. “Constraint-induced movement therapy in children with unilateral cerebral palsy.” The Cochrane database of systematic reviews vol. 4,4 CD004149. 1 Apr. 2019, doi:10.1002/14651858.CD004149.pub3
Jackman, Michelle et al. “Interventions to improve physical function for children and young people with cerebral palsy: international clinical practice guideline.” Developmental medicine and child neurology vol. 64,5 (2022): 536-549. doi:10.1111/dmcn.15055
Novak, Iona et al. “State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy.” Current neurology and neuroscience reports vol. 20,2 3. 21 Feb. 2020, doi:10.1007/s11910-020-1022-z
Stoodley, N. (2017). RCPCH clinical guideline, stroke in childhood: An evidence-based guideline for diagnosis, management, and rehabilitation. Clinical Radiology, 72. https://doi.org/10.1016/j.crad.2017.06.104
About the Author

Christina Rothfuss
Christina Rothfuss is an occupational therapy student at Southern California University of Health Sciences. She developed an interest in pediatric stroke after learning that strokes can occur in infants and children—a fact not widely known. Inspired by the important role occupational therapy plays in recovery, she is exploring how well students are prepared to support this population.
Graphics: Christina Rothfuss
Medical Editors: Manish Parakh
Junior Editor: Laila Alkhouri