by Ilona Kopyta
Childhood stroke is a challenge.
This challenge is the same in every part of the world. It can affect a patient, parent, guardian, paramedic, physician, or physiotherapist.
The first and maybe the most important point to address this problem is awareness. Stroke can happen in children!
Even people who are not part of the medical community know the warning signs of a stroke in an adults: sudden body or facial weakness, slurred speech, and difficulty with coordination or balance.
Yet, in children, these symptoms could be associated with other conditions such as encephalitis, intoxication, or trauma. The lack of awareness that a child may have a stroke can lead to delayed diagnosis. As a result, pediatric patients may not receive treatment on time. This can interfere with their education and increase their risk of chronic mental or movement disorders.
Improving social awareness of strokes in children can significantly improve children’s development and help ensure a future free from disability limitations. This is a cause worth fighting for in the media to educate society and encourage support for early intervention.
While awareness is crucial, it’s not enough to ensure proper care of a child with a suspected stroke.
If a child has acute symptoms such as paresis or slurred speech, it’s essential to bring them quickly to a hospital to perform brain imaging. However, it can be challenging to receive help in time. Ideally, the imaging protocol should involve magnetic resonance imaging (MRI) or computed tomography (CT). It is important to see the vessels of the brain.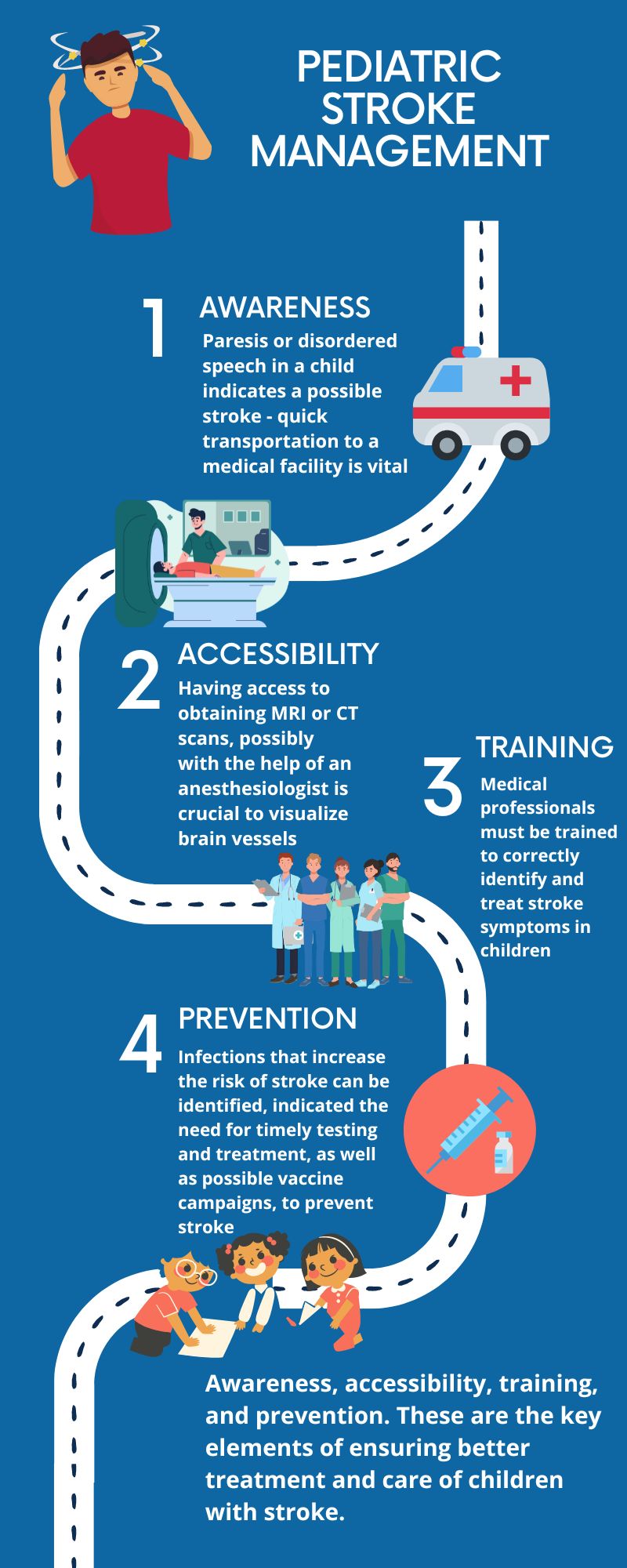
Imaging tests such as MRI or CT scans require the patient to lie down quietly. This is often hard for children. That’s why tests are typically performed under anesthesia. This means we also need access to an anesthesiologist. Since a stroke can occur at any time, we must be able to perform these tests under anesthesia at any point. Unfortunately, access to 24-hour brain imaging, particularly under general anesthesia, is rare. This problem affects healthcare systems around the world.
Let’s assume that a child with a suspected stroke goes to a hospital that can perform imaging tests at any time. Does the test alone guarantee a correct diagnosis? We must also consider the radiologist’s experience in understanding the imaging results. This can impact the accuracy of the diagnosis. It is not easy to gain such experience since pediatric stroke is relatively rare.
This brings us to the importance of training specialists in the diagnosis of children’s stroke. It’s not just radiologists who require training. Paramedics and physicians who may encounter a child with a stroke also need to understand how to recognize the symptoms and provide appropriate care. It is extremely important to include information on childhood stroke in training programs for healthcare providers.
But even if a child with a stroke is taken to a medical center that can conduct the appropriate examination, will the child receive the same level of treatment that an adult stroke patient might receive? This usually does not happen. Delayed diagnosis often results in a missed opportunity to give thrombus-dissolving treatment within the recommended time frame of 4.5 hours from the onset of symptoms. Even if a child is correctly diagnosed within this window, they are often not treated properly. This is because the center has no experience in the thrombolytic treatment of children.
Around the world, there are differences in the frequency of pediatric stroke and accessibility to care. These differences can sometimes be because of geographical variability of predisposing factors for stroke. For example, sub-Saharan African countries have a higher rate of sickle cell anemia. This is a hereditary disease leading to cerebral vascular occlusion. In some of these countries, newborns are tested for the disease to ensure treatment on time. Infections tend to be more common in developing countries. Those affecting the central nervous system are a crucial risk factor for stroke. Some of these infections can be prevented through widespread vaccination campaigns.
Awareness, accessibility, training, and prevention. These are the key elements of ensuring better treatment and care of children with stroke.
Children have always been susceptible to strokes. Despite this fact, much work remains to be done to improve their care.
Anywhere in the world.
About the Author

Ilona Kopyta, MD
Pediatric Neurology
Medical University of Silesia
Professor Ilona Kopyta is a pediatrician and specialist in child neurology, an academic teacher, a researcher and professor at the Medical University of Silesia in Katowice, Poland. Professor Ilona Kopyta completed internships abroad, among others at the Department of Child Neurology of the Royal Karolinska Hospital in Stockholm (scholarship of the “Mother and Child” Program) and the Department of Child Neurology Shaare Zedek in Jerusalem.
She is a long-time member of the International Pediatric Stroke Organization (IPSO) and the International Pediatric Stroke Study (IPSS). Professor Kopyta is the co-author of the first book in Poland to report on stroke in children, as well as Polish recommendations for the management of children with stroke.
Prof. Ilona participated in research projects devoted to her most important scientific achievement, i.e. research on risk factors for ischemic stroke in children and in cooperation with the Silesian University of Technology in Katowice in the field of engineering methods of gait testing in children with cerebral palsy treated with botulinum toxin.
Email: ilonakopyta@autograf.pl
Graphics: Sravya Jaladanki, M.D Candidate
Community Editor: Natalie Mahgerefteh & Laila Alkhouri