Homeostasis in Neonatal Stroke , The Challenges of Balance Bodily Systems in Neonatal Stroke”.
Homeostasis is the way our bodies regulate factors such as temperature, sugar levels, and blood pressure to maintain a stable internal environment. Think of a thermostat that turns on the heat when a room gets too cold and turns it off when the room reaches the right temperature. Our bodies have many similar mechanisms. When talking about neonatal stroke, helping a baby maintain homeostasis may be important in helping the brain recover as best it can.
Neonatal Stroke and Homeostasis
A neonatal stroke happens when the blood flow to part of the newborn’s brain is blocked within the first 28 days of life. This interruption in blood flow can be caused by factors such as blood clots, broken blood vessels, or complications of a premature birth. The resulting ischemia (lack of blood supply) can lead to cell death, inflammation, and long-term neurological and developmental problems. Homeostasis in the newborn is essential in such cases to lower the effects of the stroke and promote recovery.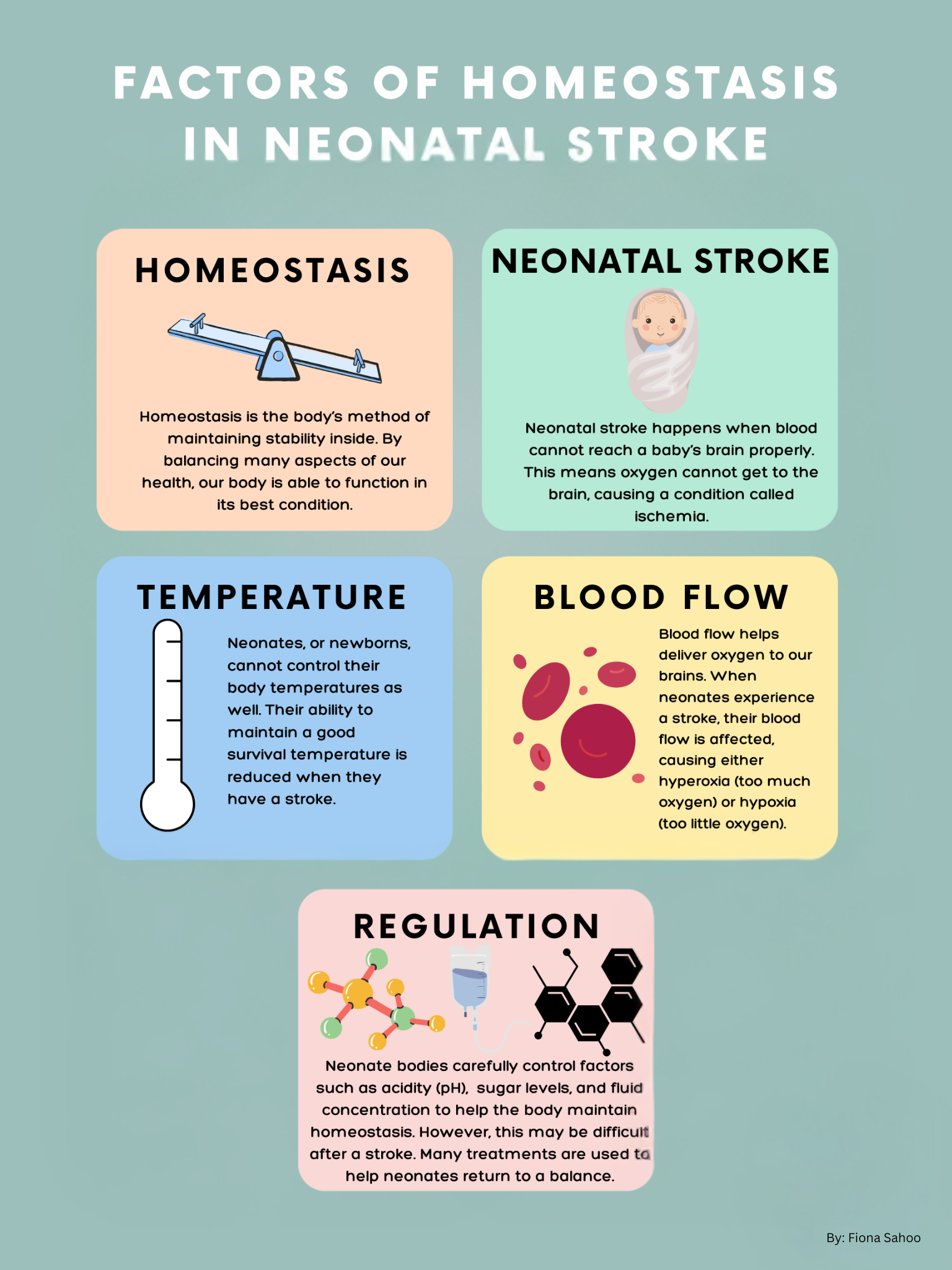
Key Aspects of Homeostasis in Neonatal Stroke:
- Excessive brain activity: Seizures
- Overactivity of the brain in the form of seizures is very common in neonatal stroke. Medications to limit seizure activity may help the brain rest and reduce the injury caused by stroke.
- Temperature Regulation:
- Neonates (newborns) cannot control their body temperature as well. It is important to keep the baby’s body temperature within a normal range (around 36.5–37.5°C) which may help to minimize the initial injury of a stroke.
- Oxygenation and Blood Flow:
- Oxygen and nutrients must reach the brain to prevent more cell damage and help recovery. Neonates may need supplemental oxygen (treatment to provide extra oxygen) or other respiratory support to manage blood oxygen levels carefully.
- Close monitoring of blood pressure is important because hypotension (low blood pressure) can increase an ischemic injury.
- Glucose Homeostasis:
- Neonates, especially preterm infants, are more prone to hypoglycemia (low blood sugar). This can lower brain function and recovery after a stroke. Strokes may also disrupt the brain’s ability to use glucose (sugar) properly. Therefore, blood glucose levels are checked to get the correct levels, especially during the critical period after a stroke.
- Fluid and Electrolyte Balance:
- Maintaining appropriate levels of fluids and electrolytes (such as sodium, potassium, and calcium) is necessary in neonatal stroke. Fluid therapy may be used to fix this.
Challenges in Maintaining Homeostasis After Neonatal Stroke
- Limited Reserve in Neonates: Neonates are not fully developed human beings. This means their bodies may have a harder time correcting imbalances.
- Difficulties in Monitoring: Neonates are small and often fragile, making monitoring factors like blood pressure, oxygen saturation, and glucose levels challenging. Brain monitoring is often used to detect seizures and guide the use of antiseizure medications.
- Increased Susceptibility to Secondary Injury: Neonates may experience secondary complications like seizures, which can further impair brain function.
Approaches For Treatment and Neuroprotection
The main goal in treating a newborn after a stroke is to stabilize their condition, keep their body balanced, and prevent further harm. Common interventions include:
- Seizure monitoring and management and prevention of further neurological damage
- Oxygen supplementation or mechanical ventilation to ensure adequate oxygenation
- Fluid management and monitoring of electrolytes
- Glucose control, especially in the case of hypoglycemia
Conclusion
Homeostasis is important in caring for neonates who have experienced a stroke. Effective management of seizures, temperature, oxygenation, blood pressure, and glucose, may help reduce further brain injury and optimize recovery. The delicate and complex nature of a newborn’s body makes maintaining homeostasis during and after a stroke essential, requiring careful monitoring to protect the brain and optimize outcomes.
About the Author

Yasmin Aly Farid
Dr. Yasmin Aly Farid is an Assistant Professor of Pediatrics and Neonatology at Ain Shams University (ASU) and an International Board-Certified Lactation Consultant (IBCLC). A member of the Royal College of Pediatrics and Child Health (RCPCH), they previously served as Director of the NICU at ASU Children’s Hospital. She is also a founder of the Ain Shams Society for Neonatal Care & CME, contributing to neonatal care, medical education, and research.
Graphics: Fiona Sahoo
Medical Editor: Janette Mailo, MD, PhD, FRCPC
Junior Editor: Fiona Sahoo