Hemorrhagic Strokes in Neonates
A sudden bleed in the brain is called a hemorrhagic stroke. This type of stroke is more common in babies born prematurely (before 32 weeks), but it can also happen in full-term babies. Doctors call it a perinatal stroke if it happens within the first 28 days of life, and a childhood stroke if it happens later, up to age 18. According to the American Stroke Association (Ferriero et al., 2019), about 20% of perinatal strokes are due to bleeding, also known as hemorrhage, affecting around 6 in every 100,000 live births.
Some known risk factors (Bruno et al., 2014) include severe heart abnormalities developed while inside the womb and fetal distress during childbirth. However, there is not much that is known about the causes, and outcomes can be very different from baby to baby. Some may present as seizures, with sudden stiffness and jerking of the body, or may be non-specific and include symptoms like fever or lethargy.
For these infants, it is imperative to do the proper imaging studies, rule out other causes of presentation, and manage appropriately.
The American Stroke Association also provides a summary of perinatal stroke available at https://www.stroke.org/en/about-stroke/stroke-in-children/perinatal-stroke-infographic.
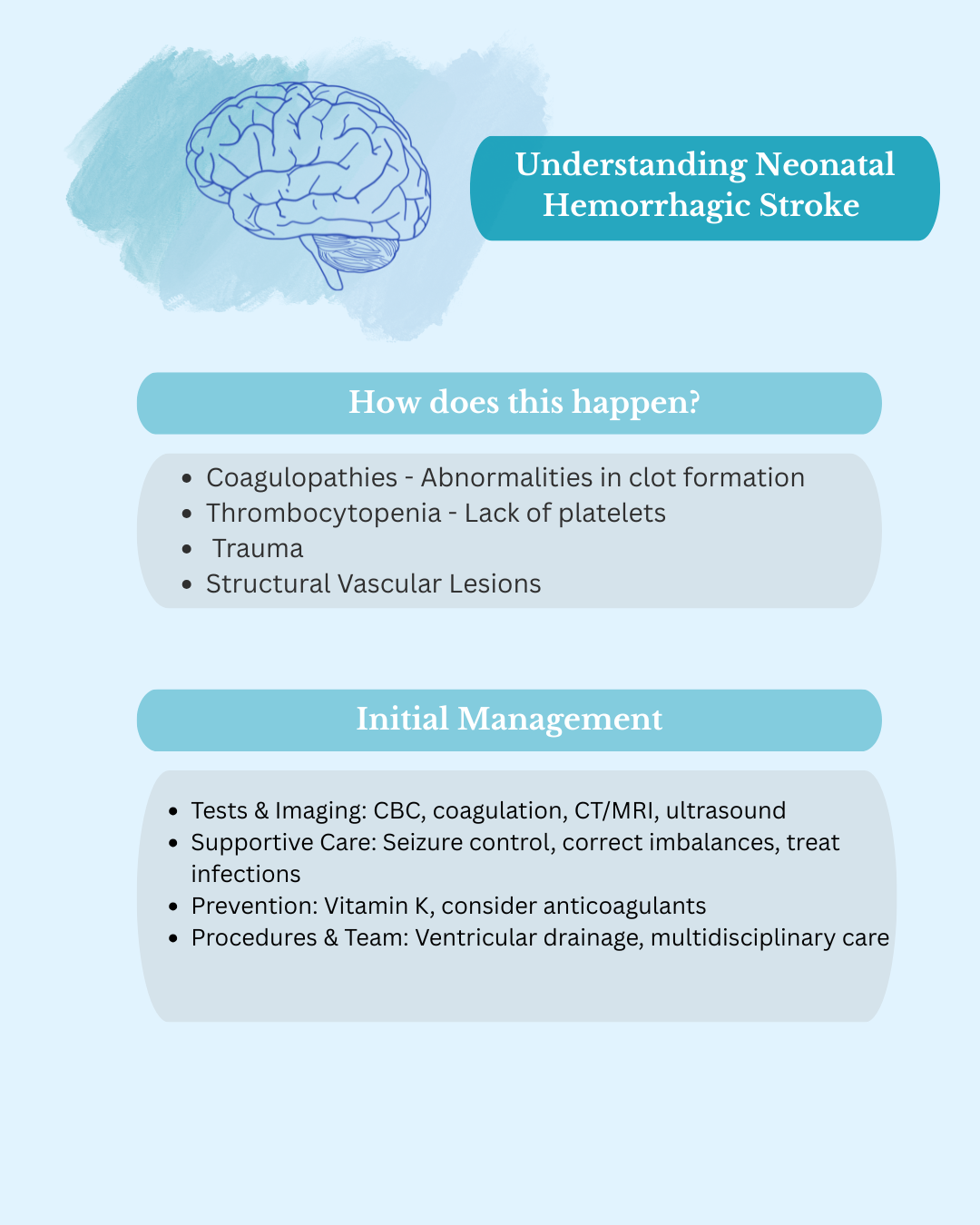
How does this happen?
The exact causes of hemorrhagic stroke in newborns are poorly understood, but there are some common mechanisms which include:
- Coagulopathies- Abnormalities in clot formation, notably due to vitamin K deficiency
- Thrombocytopenia- Lack of platelets which are necessary for formation of clots
- Structural Vascular Lesions- Abnormalities in blood vessel supply to the brain
In some cases, there is a blockage in one of the blood vessels supplying blood to the brain, which leads to an ‘infarct’, or a tissue that lacks blood supply. This is known as an ischemic stroke. This causes the blood vessels to become damaged and start bleeding, leading to a hemorrhagic stroke. This commonly occurs in the blood vessels known as the Cerebral Venous Sinus, and when it occurs here, it is referred to as Cerebral Venous Sinus Thrombosis (CVST).
Hemorrhagic stroke can occur in different parts of the brain, such as the ventricles (fluid-filled spaces within the brain), in the parenchyma (the brain tissue itself) or in the spaces between the meninges (the layers covering and cushioning the brain).
Initial Management of Neonatal Hemorrhagic Stroke
Initial management of neonatal hemorrhagic stroke begins with tests such as complete blood counts, lumbar puncture, and blood studies including coagulation. Imaging tests often start with a CT scan of the brain, followed by MRI or special scans of blood vessels if needed. Cranial ultrasound is also very important at times when a CT scan cannot be done quickly or safely. These tests help confirm the diagnosis, show how severe the bleeding is, guide treatment, and allow doctors to track progress. Electroencephalography (EEG) can also be used to check brain activity and record seizures.
Contrary to adult stroke, there is no established definitive treatment for perinatal stroke, other than management of symptoms. Therefore, a multidisciplinary team consisting of neonatology, pediatric neurology, hematology, radiology, and so on is involved in providing care for the patient.
There are many considerations mentioned by the American Stroke Association:
- Supportive measures such as control of seizures, correction of electrolyte abnormalities and treatment of underlying infections
- Routine administration of vitamin K to newborns to prevent hemorrhage and correct deficiencies
- Consideration of blood thinners such as aspirin, Low Molecular Weight Heparin or Unfractionated Heparin in newborns who are at risk of recurrence of stroke to prevent an ischemic event such as CVST
- In cases of IVH with hydrocephalus or elevated intracranial pressure, ventricular drainage may be considered
Outcomes and Considerations
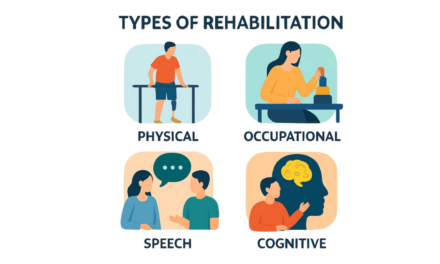
Neurological outcomes can be favorable in select cases managed conservatively. However, serious outcomes like disability or even death can still occur, depending on the severity, location, and underlying cause of the stroke. As a result, it is always important to discuss with the multidisciplinary team when considering short-term and long-term rehabilitation plans.
Over time, treatment must be personalised for each child. This may involve physiotherapy, occupational therapy, speech and language therapy, and/or social workers. It is also imperative for parents and caregivers to work with the medical team to support their child’s care.
References:
Ferriero DM, Fullerton HJ, Bernard TJ, Billinghurst L, Daniels SR, DeBaun MR, deVeber G, Ichord RN, Jordan LC, Massicotte P, Meldau J, Roach ES, Smith ER; American Heart Association Stroke Council and Council on Cardiovascular and Stroke Nursing. Management of Stroke in Neonates and Children: A Scientific Statement From the American Heart Association/American Stroke Association. Stroke. 2019 Mar;50(3):e51-e96. doi: 10.1161/STR.0000000000000183. PMID: 30686119.
Bruno CJ, Beslow LA, Witmer CM, Vossough A, Jordan LC, Zelonis S, Licht DJ, Ichord RN, Smith SE. Haemorrhagic stroke in term and late preterm neonates. Arch Dis Child Fetal Neonatal Ed. 2014 Jan;99(1):F48-53. doi: 10.1136/archdischild-2013-304068. Epub 2013 Aug 30. PMID: 23995383; PMCID: PMC3864979.
Basu AP. Early intervention after perinatal stroke: opportunities and challenges. Dev Med Child Neurol. 2014 Jun;56(6):516-21. doi: 10.1111/dmcn.12407. Epub 2014 Feb 17. PMID: 24528276; PMCID: PMC4020312.
Gupta SN, Kechli AM, Kanamalla US. Intracranial hemorrhage in term newborns: management and outcomes. Pediatr Neurol. 2009 Jan;40(1):1-12. doi: 10.1016/j.pediatrneurol.2008.09.019. PMID: 19068247.
About the Author

Esha Parakh
Birmingham, UK
Graphics: Neha Ramiah
Medical Editors: Shelley Dean
Junior Editor: Neha Ramiah