Going back to school after a stroke is an important event! To make the transition easier for your child and reduce stress, you need to communicate well with your child’s school.
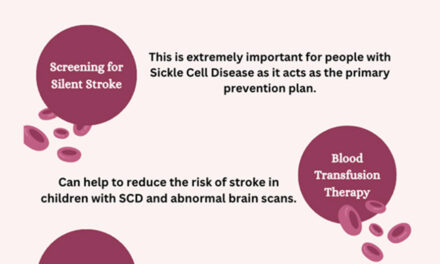
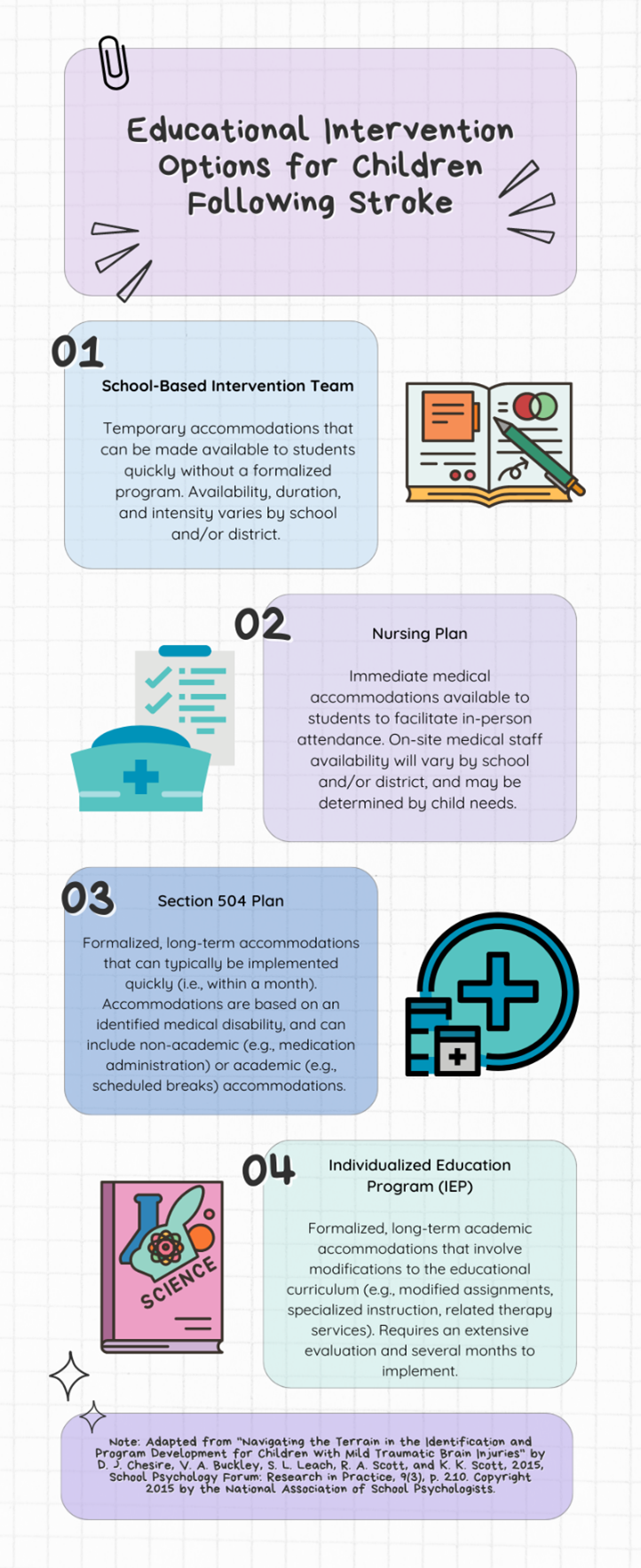
Tell the school team, which includes teachers, the principal, the school psychologist, or the nurse, all about your child’s medical condition and recovery. You can get a letter from your child’s doctors with key details for the school. When you give this letter to the school, you might want to send a note or set up a meeting. During this meeting, ask the team to create a plan to support your child. The kind of help your child needs can be different at each school. Everyone on your child’s team, including you, should get regular updates on how your child is doing. This helps make sure they are getting what they need and lets the team make any needed changes. Remember, you know your child best, so do not be afraid to speak up for what you think they need. You can find more information in the infographic.
There is no set time for your child to go back to school after a stroke. The timeline will be set and watched by your child’s medical team based on symptoms and treatment needs. But while waiting to go back to school, your child can stay connected with classmates. This could mean video-calling during a class event, saying hello in class, going to school events, or visiting friends outside of school, if possible.
Once cleared medically to begin going back to school, it is best to start slowly. Begin with just a few hours each day, only a few days a week. Listen to your child and what they feel up to, but also encourage them to try. Then, little by little, your child can work up to longer school days. It is important for your child to have breaks, both in and out of the classroom (like in the nurse’s office), whenever they need to rest while at school. Once again, there is no set plan for how your child should go back to school after a stroke. The whole team, including doctors, teachers, and family, should keep a close eye on it.

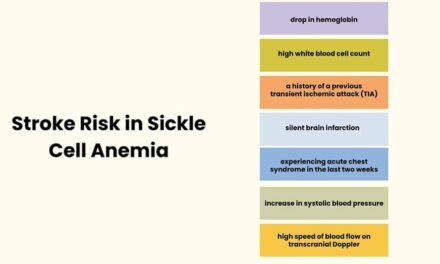
After a stroke, students have new learning needs. Your child may experience a level of symptoms: physical changes (like feeling tired more easily, having trouble with movements, or changes in vision), cognitive challenges (such as hard time focusing, learning new information, language changes), emotional changes (such as worrying more, feeling sadder, or having less patience), and social challenges (such as getting along with classmates, missing out on hobbies they used to enjoy, or feeling left out of activities they can’t join).
It is a good idea to involve your child in planning their support and changes in how they learn. This can help them figure out what works best for them and when to ask for help. It can also make them more willing to use helpful interventions. Keep in mind, the support your child needs depend on the physical changes from the stroke and any hidden changes in how they think, feel, and act. See the infographic for ideas on how to help your child in these areas.
Resources:
- https://www.stroke.org.uk/resources/supporting-children-after-stroke-toolkit-teachers-and-childcare-professionals
- https://www.pta.org/home/family-resources/Special-Education-Toolkit/Special-Education-Toolkit-Resources#:~:text=Parent%20Training%20and%20Information%20Centers,locate%20one%20in%20your%20state.
- https://www.parentcenterhub.org/tbi/#parents
- https://www.braininjuryaustralia.org.au/wp-content/uploads/TBI_School_after_TBI.pdf
- https://chasa.org/school/
About the Author

Lauren Demers, PhD
Pediatric Neuropsychology
Dr. Lauren Demers is a psychologist resident (emphasis in pediatric neuropsychology) at Oregon Health & Science University in Portland, Oregon where she sees children with neurological conditions and injuries, including stroke, in the Pediatric Critical Care and Neurotrauma Recovery Program. She will be joining the faculty at Children’s Hospital of Philadelphia this fall.

Eleanor Bold, MA
Pediatric Psychology
Eleanor Bold is a doctoral intern in pediatric psychology at Oregon Health & Science University in Portland, Oregon where she sees children with neurological conditions and injuries, including stroke, in the Pediatric Critical Care and Neurotrauma Recovery Program. She will be starting a post-doctoral fellowship in pediatric rehabilitation psychology at Children’s Hospital Colorado this fall.
Medical Editor: Gayatra Mainali, MD
Community Editor: Jalaia Jackson