Family-centered care is a way of providing healthcare where the family is an important part of the patient’s recovery. Family is not just a helper. For pediatric stroke (a stroke that happens to a child), this approach is especially important. Children who have had a stroke may need help for a long time. Their families are usually the ones providing daily care. This means families play a big role in medical treatment, ongoing therapy, and emotional support.
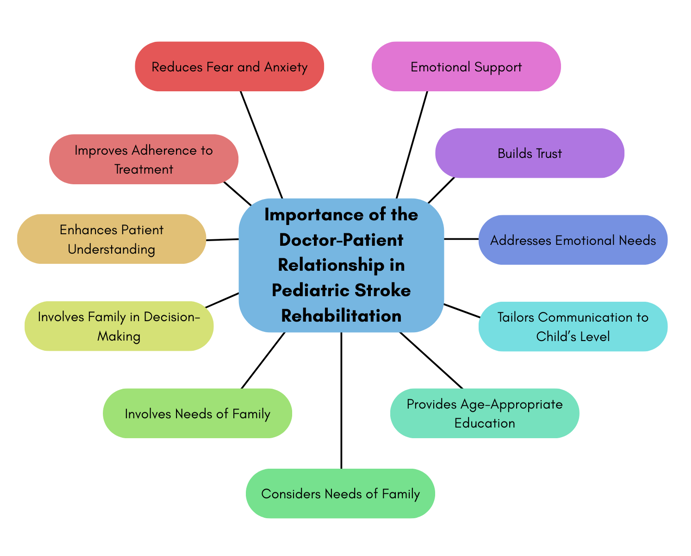
Three Main Parts of Family-Centered Care
1. Good Communication – Patients, families, doctors, and therapists should share information clearly and regularly.
2. Teamwork – Families and healthcare teams work together. They set goals, check progress, and change treatment plans when needed.
3. Long-term Relationships – Recovery can take months or years. Families and healthcare teams need to build trust. They also need to stay connected throughout the process.
Pediatric Stroke – What It Means
A pediatric stroke happens when a blood vessel in a child’s brain is blocked or bursts. This causes a brain injury. Treating children is different from treating adults. Providers must think about the child’s growth, development, and long-term future. Care must help the child heal while also supporting learning, emotions, and social life.
Why Family-Centered Care Matters
Children often rely on their families for daily care. Families play a huge role throughout recovery.
Challenges in Family-Centered Care
– Communication Problems – Families may not understand medical terms. Sometimes they may speak another language. This can make it hard to share important information.
– Coordinating Specialists – Pediatric stroke care often involves many specialists. This can make scheduling and sharing updates more challenging.
– Maintaining Long-term Care – Changes in staff, resources, or family situations can disrupt care.
– Resources – Extra training, tools, and support take time and money. Sometimes these can be hard for hospitals to provide. Pediatric stroke places a significant economic and emotional burden on caregivers, often requiring changes in employment or lifestyle to manage post-stroke rehabilitation needs (Aprile et al., 2025).
Opportunities in Family-Centered Care
– Happier Patients and Families – When families are part of care decisions, they feel more respected. This makes them more likely to follow treatment plans.
– Better Care and Outcomes – Good communication and teamwork lead to better emotional and medical results.
– New Ideas and Technology – Working with many specialists can bring new ways to deliver care. Telehealth is a good example of this. This lets providers see and evaluate patients using the internet.
– Learning Together – Families and healthcare teams can learn from each other’s experiences. This can help to improve care over time.
How to Put Family-Centered Care into Action
– Check the family’s strengths, needs, and resources regularly—not just once.
– Set realistic goals together with the family.
– Create home exercise programs that fit the child’s needs and the family’s abilities.
– Teach and train caregivers so they feel confident providing care.
– Keep in touch regularly and answer questions quickly.
– Check the home environment for anything that might make recovery harder.
In Summary
Recovering from a pediatric stroke can be a long and complex journey. Family-centered care can make recovery more effective and caring. It uses good communication, teamwork, and long-term relationships. It is important for families and healthcare teams to work together. This way, children not only survive, but thrive.
Family-Centered Care Visualization Table
| Key Area | What It Means | For Parents |
| Communication | Clear and regular sharing of information between families, doctors, and therapists. | Ask questions, repeat what you understand, and request simpler terms if needed. |
| Teamwork | Families and healthcare teams work together to set goals and change treatment when needed. | Take part in setting goals, attend meetings, and share your child’s progress and concerns. |
| Long-term Relationships | Building trust and staying connected for months or years of recovery. | Stay in touch with main care providers and keep notes of your child’s progress. |
| Challenges | Barriers to understanding, coordinating many specialists, maintaining care, and dealing with limited resources. | Speak up if something is unclear, and ask for help with scheduling appointments. |
| Opportunities | Happier families, better quality care, new technical solutions, and learning together. | Join support groups, explore telehealth, and give feedback to improve care. |
| Action Steps | Check family’s needs, set realistic goals, create home programs, train caregivers, stay connected, and check home environment. | Work with your healthcare teams to make a plan you can follow at home and change when needed. |
About the Author

Shelley A. Dean, OTD, MBA, OTR/L
Dr. Shelley Dean is an occupational therapist with nearly 30 years of experience specializing in pediatrics. She holds a post-professional Doctorate in Occupational Therapy from Quinnipiac University and a Master’s in Occupational Therapy from Washington University in St. Louis. Dr. Dean is also an MBA candidate at Queens University in Charlotte. She is the founder of Crossway Pediatric Therapy, where her team provides comprehensive therapy services to children with special needs.
Dr. Dean has pioneered the treatment of pediatric stroke, hosting internationally attended constraint-induced movement therapy intensives. She serves on the board of the International Alliance for Pediatric Stroke and is a charter member of the International Pediatric Stroke Organization, contributing to research, clinical practice, and parent training in the field. She is also a mentor and educator, dedicated to advancing the knowledge and skills of future therapists.
Outside of her professional work, Dr. Dean enjoys reading, walking her dog, and spending time with her family in Charlotte, where she lives with her husband Doug and their blended family.
Graphics: Shelley A. Dean, OTD, MBA, OTR/L
Medical Editors: Kevin O’Connor
Junior Editor: Jeehyun Kim