Authors: Esha Parakh and Claire Champigny
Objective:
To review post-stroke outcomes, including neurocognitive impairments, mental health challenges, sensory-motor difficulties, and epilepsy. Sequelae means the long-term conditions that happen because of an illness or injury.
What is a stroke?
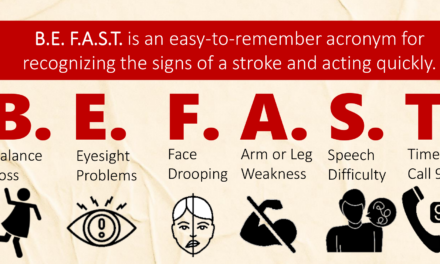
A stroke occurs when the blood supply to the brain is interrupted. It could be due to a blockage of the blood vessel (ischemic stroke) or bleeding (hemorrhagic stroke). Stroke occurs in about 2.5 to 13 children per 100,000. Therefore, it is essential that we quickly recognize the signs of stroke and initiate prompt treatment. A timely response can impact treatment efficacy and improve recovery and outcomes.
What are post-stroke consequences?
Stroke consequences can be temporary or permanent, and some may even first appear years after the stroke. About 60-70% of children with stroke experience a long-term disability.
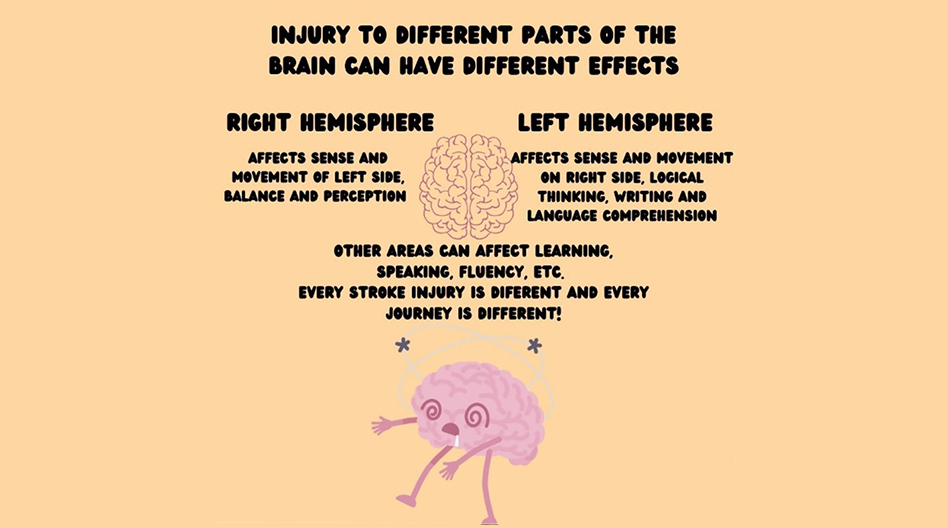
Stroke consequences result from damage to the part of the brain that controls certain functions that become affected by the stroke. The brain area and the network connections that are impacted influence the outcome.
It is also important to remember that a stroke can occur again, and how often that happens depends on what initially caused the stroke. For example, if the problem is abnormal blood vessels, the chance of having a stroke in 5 years can be as high as 66%. Therefore, it is crucial to be aware of the primary cause by discussing it with a doctor and undergoing proper investigations, treatment and management.
Some expected post-stroke consequences are discussed below.
Neurocognitive Deficits
The effects of a stroke depend on multiple factors, such as the location of the stroke, the extent of the injury, other problems caused by the stroke (e.g., hydrocephalus, edema), and other medical details that can be determined through imaging and thorough discussion with the medical team. Non-clinical factors, such as socioeconomic status, have also been associated with stroke outcomes.
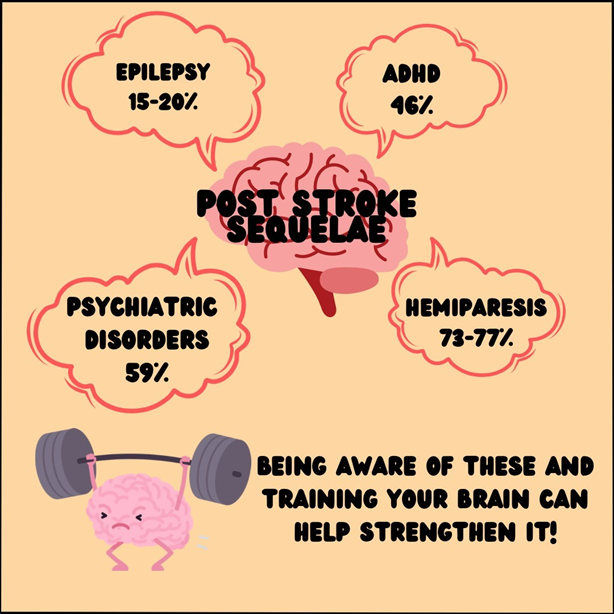
Epilepsy is commonly seen when there is an injury to the temporal lobe of the brain. Epilepsy is a condition in which recurring seizures occur. About 15-20% of children who experience an ischemic stroke and over 17% who experience a hemorrhagic stroke develop post-stroke epilepsy.
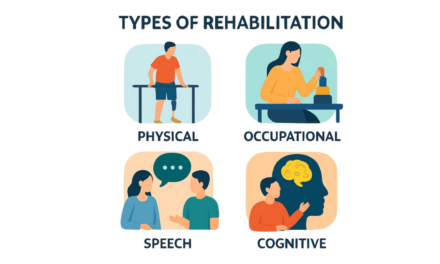
Verbal skills and language comprehension may also be impacted (aphasia), and children may require speech therapy.
Around 46% of children with stroke develop ADHD (Attention-Deficit/Hyperactivity Disorder), and around 41% are diagnosed with a learning disorder.
Children who experience a stroke before the age of 1 show an increased risk of intellectual impairment, and about 10% of youth with perinatal stroke will be diagnosed with intellectual disability.
Mental Health
Experiencing a stroke is a traumatic event, and the recovery can be challenging. 59% of children with stroke develop a psychiatric disorder. Specifically, pediatric stroke is linked with a high prevalence of anxiety disorder (31%), mood disorders (21%), and personality changes (17%).
Sensory-Motor Disability
Depending on the severity and characteristics of the stroke, there can be a wide range of motor problems, such as weakness (hemiparesis) and paralysis (hemiplegia) of one-half of the body. Overall, about 50 to 80% of children with stroke will develop long-term motor disability. The most common is hemiparesis, present in 73-77% of children with ischemic stroke. Other motor impairments, including dystonia (uncontrollable muscle contractions), spasticity (muscle tightness), and ataxia (loss of coordination and muscle control) or sensory changes, are often present in isolation or combination.
References
- Rawanduzy CA, Earl E, Mayer G, Lucke-Wold B. Pediatric Stroke: A Review of Common Etiologies and Management Strategies. Biomedicines. 2022 Dec 20;11(1):2. doi: 10.3390/biomedicines11010002. PMID: 36672510; PMCID: PMC9856134.
- Tsze DS, Valente JH. Pediatric stroke: a review. Emerg Med Int. 2011;2011:734506. doi: 10.1155/2011/734506. Epub 2011 Dec 27. PMID: 22254140; PMCID: PMC3255104
- Kopyta I, Sarecka-Hujar B, Raczkiewicz D, Gruszczyńska K, Machnikowska-Sokołowska M. Assessment of Post-Stroke Consequences in Pediatric Ischemic Stroke in the Context of Neuroimaging Results-Experience from a Single Medical Center. Children (Basel). 2021 Apr 8;8(4):292. doi: 10.3390/children8040292. PMID: 33917968; PMCID: PMC8068320.
- Krivitzky LS, Westmacott R, Boada R, Sepeta L, Reppert L, Mrakotsky C. Recent Advances in Neuropsychological Outcomes and Intervention in Pediatric Stroke. Stroke. 2022 Dec;53(12):3780-3789. doi: 10.1161/STROKEAHA.122.037294. Epub 2022 Oct 11. PMID: 36252123.
- Fullerton HJ, Wintermark M, Hills NK, Dowling MM, Tan M, Rafay MF, Elkind MS, Barkovich AJ, deVeber GA; VIPS Investigators. Risk of Recurrent Arterial Ischemic Stroke in Childhood: A Prospective International Study. Stroke. 2016 Jan;47(1):53-9. doi: 10.1161/STROKEAHA.115.011173. Epub 2015 Nov 10. PMID: 26556824; PMCID: PMC4696877.
- Greenham M, Gordon A, Anderson V, Mackay MT. Outcome in Childhood Stroke. Stroke. 2016 Apr;47(4):1159-64. doi: 10.1161/STROKEAHA.115.011622. Epub 2016 Mar 8. PMID: 26956257.
- Sundelin HE, Tomson T, Zelano J, Söderling J, Bang P, Ludvigsson JF: Pediatric ischemic stroke and epilepsy: a nationwide cohort study. Stroke. 2021, 52:3532-40. 10.1161/STROKEAHA.121.034796
- Champigny CM, Deotto A, Westmacott R, Dlamini N, Desrocher M. Academic outcome in pediatric ischemic stroke. Child Neuropsychol. 2020 Aug;26(6):817-833. doi: 10.1080/09297049.2020.1712346. Epub 2020 Jan 9. PMID: 31914852.
- Max JE, Mathews K, Lansing AE, Robertson BA, Fox PT, Lancaster JL, Manes FF, Smith J. Psychiatric disorders after childhood stroke. J Am Acad Child Adolesc Psychiatry. 2002 May;41(5):555-62. doi: 10.1097/00004583-200205000-00013. PMID: 12014788.
- Williams TS, McDonald KP, Roberts SD, Dlamini N, deVeber G, Westmacott R. Prevalence and Predictors of Learning and Psychological Diagnoses Following Pediatric Arterial Ischemic Stroke. Dev Neuropsychol. 2017;42(5):309-322. doi: 10.1080/87565641.2017.1353093. Epub 2017 Aug 14. PMID: 28805445.
About the Author

Esha Parakh
Birmingham, UK

Claire Champigny
Toronto, Canada
Medical Editors: Janette Mailo, MD
Junior Editor: Sanjana Sivakumar