Author: Sravya Jaladanki
Disclaimer: This article discusses the steps emergency medical services (EMS) personnel can take to identify pediatric stroke and how medics can assist patients before they reach the hospital. This article may be triggering to families of children with stroke.
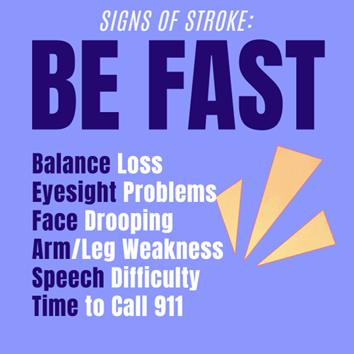
Parents, teachers, caregivers, and so forth should know the acronym “B.E.F.A.S.T” to help remember the signs of stroke and identify if someone is having a stroke:
- Balance loss
- Eyesight problems
- Face drooping
- Arm/leg weakness
- Speech difficulty
- Time to call 911
Age is an important factor when it comes to stroke symptoms. Children that are < 6 years of age will more often present with altered mental status and seizures. Children may also present with hemiparesis (half the body has muscle weakness or is paralyzed), and aphasia (difficulty speaking, writing, and/or understanding spoken/written language). Headache, vomiting, loss of balance, and sudden change in vision, are all potential symptoms as well. In most cases, the symptoms come on very suddenly. Symptoms that come on gradually, over hours or days, are less likely to be related to stroke. If your child is experiencing any of the above signs, it is recommended to lay your child down flat to help with blood flow.
Time is of the essence when dealing with stroke patients, including pediatric patients. Ideally, every child suffering from a stroke would begin receiving treatment immediately. Although it can be an extremely scary and a tense situation, it is important to remain calm and follow proper protocol to get help. But what are these steps?
Protocols may vary from hospital to hospital but often remain similar. Here are typical steps for EMS personnel:
- As soon as a call is received about a possible stroke, EMS is dispatched to the scene.
- Once EMS arrives on the scene, a brief history of events will be collected as well as the patient’s medical history.
- The team will immediately determine if the child needs help with their breathing.
- If the patient is experiencing a seizure, appropriate medication will be given per the discretion of the health care providers.
- Intravenous lines (IVs) are placed and a normal saline bolus (rapidly administering a single, large dose of saline into the vein) is given.
- EMS will try to keep the patient normothermic (normal body temperature) and normotensive (normal blood pressure) while transport protocols to the hospital are started.
EMS has the crucial job of keeping the patient stable until they reach the hospital. However, it is also important to discuss how they can help identify stroke symptoms in a pediatric patient, as research has shown that diagnosis time can be delayed and as high as 24 hours or more in some instances.
The National Institutes of Health (NIH) has also created a stroke scale for stroke patients which can be used to assess the severity of a stroke. A modified version of the stroke scale is applied to pediatric patients. Questions are asked to assess level of consciousness and the child is asked to follow various commands that will indicate if there is any type of weakness or paralysis. The scale ranges from a score of 0 to 42, with 42 being the most severe stroke symptoms. This score can help clinicians determine if a stroke is occurring and help guide management.
Emergency Services are extremely important, as they are the first ones to provide life-saving care for a child experiencing a stroke. For this reason, pediatric stroke symptoms must be clearly understood, along with the general stroke protocols. This will ensure that every child is helped as soon as possible and is set up for the best possible outcomes. Remember, Time is Brain!
About the Author
Sravya Jaladanki
M.D. Candidate
Sravya Jaladanki is a third year medical student at Northeast Ohio Medical University and has a Bachelor’s degree in Political Science and minor in Global Health from UCLA. She is planning on specializing in the field of anesthesiology and is especially interested in working with the pediatric population. She is also interested in research, and has ongoing projects in pediatric anesthesiology and orthopedic surgery at Akron Children’s Hospital and UCSF. She is currently working towards her MBA through the University of Akron, and hopes to use the practical and interpersonal skills she will gain through the program in order to bring a unique perspective to the increasingly complex healthcare landscape. Sravya hopes to explore her personal and professional interests through the rest of her time in medical school, and in her spare time enjoys writing, cooking, and spending time with family and friends.
Medical Editors: Fiza Laheji, MD
Junior Editor: Sanjana Sivakumar and Karen Glenn