Author: Rabia Qaiser, MD
Introduction:
In the US, pediatric strokes happen in about 2.5 to 13 out of every 100,000 kids each year. Strokes in children can lead to serious problems that might need surgery, like severe brain swelling and hydrocephalus (fluid buildup in the brain). Catching these issues early can help save lives and manage complications. This article will discuss the need for two types of surgery: decompressive hemicraniectomy and treatment for hydrocephalus.
Nonsurgical management of Stroke:
Doctors can treat strokes without surgery using medicines like intravenous tissue plasminogen activator (tPA) and a procedure called mechanical thrombectomy. They also manage brain
swelling with medications, controlling sodium levels, sedatives, and managing blood carbon dioxide levels.
Neurosurgical Management of Cerebral Edema:
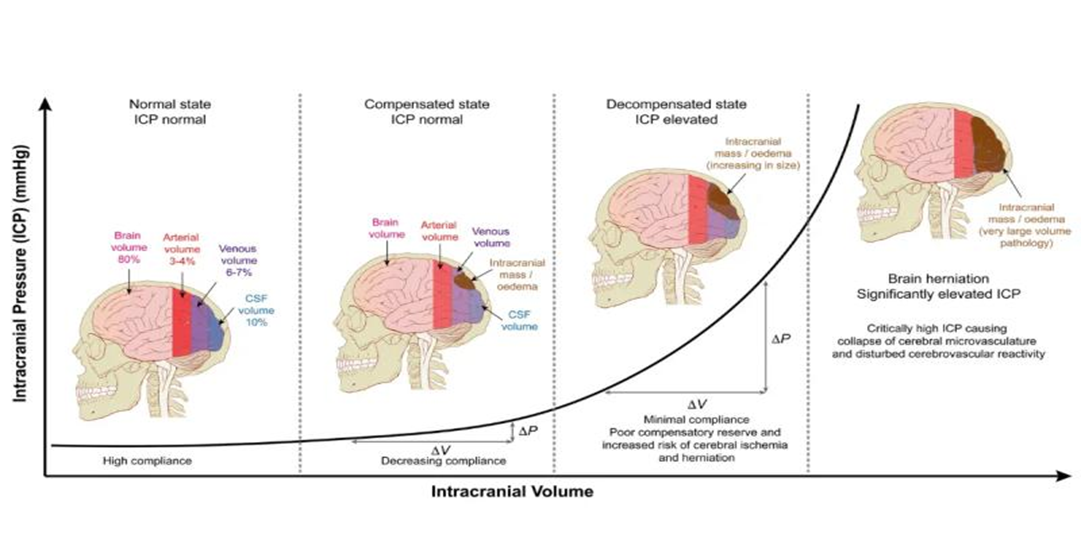
Figure 1. The Monro-Kellie hypothesis: applications in CSF volume depletion (Mokri, 2001)
The intracranial volume-pressure curve (1) No pathology (2) Small volume pathology in a compensated state with normal ICP (3) Large volume pathology in a decompensated state with elevated ICP (4) Very large volume pathology with a significantly elevated ICP and brain herniation https://teachmesurgery.com/neurosurgery/flow-and-pressure/monro-kellie-doctrine/
A stroke can cause the brain to swell. Since the skull encases the brain, cerebrospinal fluid, and blood, any increase in one of these components can cause dangerous elevations in the pressure in the skull. This can push the brain out of its normal position, a serious condition known as “herniation.” This is explained by the “Monro-Kellie Doctrine” (see figure 1) reference.
Doctors first try to control swelling with medication. If swelling continues to increase and the pressure rises, a procedure called “hemicraniectomy” might be needed. This involves removing a large part of the skull to allow the brain to swell without causing herniation. Once the swelling goes down, the skull piece is put back. Studies show that while hemicraniectomy can help adults, there is less information about its effects on children. One study found an 8% death rate for children after this surgery. In contrast, 12% of older adults who had the surgery were able to live independently, while 80% were either disabled or died (see reference 3).
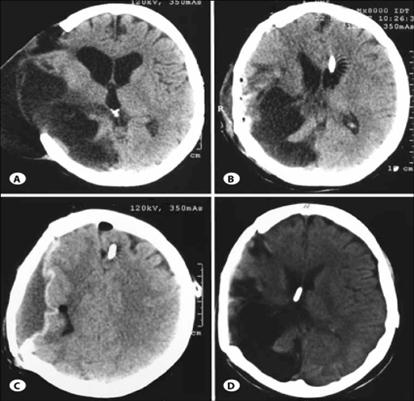
Figure 2. Head CT showing Hemicraniectomy with brain herniation (A) and Hydrocephalus with shunt catheter (B, C & D)
Management of Hydrocephalus:
Hydrocephalus, or fluid buildup in the brain, can also happen after a stroke (see figure 2). There isn’t much information about hydrocephalus in children who have had strokes, but in general, about 1% of kids with brain injuries develop hydrocephalus (see references 4 and 5).
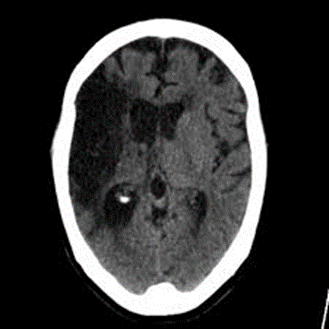
Figure 3. Ventriculoperitoneal shunt showing a ventricular catheter, valve and peritoneal catheter
To treat this, doctors often use a ventriculoperitoneal shunt. This device has three parts: a catheter Epilepsy is commonly seen when there is an injury to the temporal lobe of the brain. Epileps that drains into the abdominal cavity. The shunt is usually made from silicon (see figure 3). It’s important to distinguish between hydrocephalus that happens because the brain has shrunk (“Hydrocephalus ex vacuo,” see figure 4) and hydrocephalus due to poor fluid absorption. Only the latter needs a shunt. Signs of shunt problems include headaches, nausea, vomiting, unusual eye movements, drowsiness, or swelling near the shunt. If any of these occur, patients should see a neurosurgeon right away.
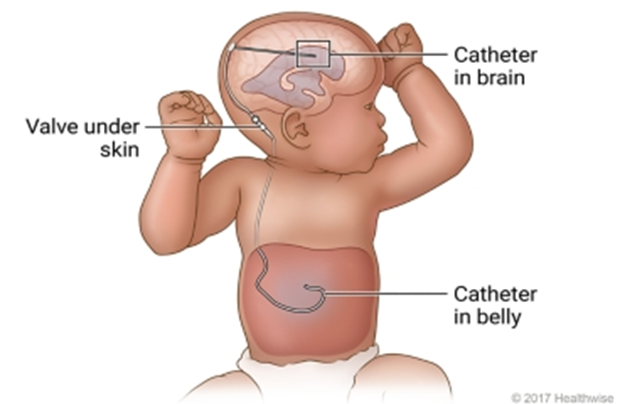
Figure 4. Head CT showing hydrocephalus ex vacuo
Conclusion:
Stroke is a serious issue that affects more children than we might realize. Early detection and proper management of acute stroke can help reduce the risks and improve outcomes for these young patients.
References
-
- Aging Dis. 2021 Jul; 12(4): 1043–1055. Published online 2021 Jul 1. doi: 10.14336/AD.2021.0219 PMCID: PMC8219494 PMID: 34221548 Pediatric Stroke: Overview and Recent Updates Mary Hollist, Katherine Au, Larry Morgan, Padmashri A Shetty, Riddhi Rane, Abraham Hollist, Angela Amaniampong and Batool F Kirmani
- J Child Neurol. 2019 Oct;34(12):765-769.doi: 10.1177/0883073819855534. Epub 2019 Jul 8.
Characteristics and Outcome in Children With Craniectomy Following Acute Ischemic Stroke in the International Pediatric Stroke Study. Laura L Lehman, Gabrielle DeVeber, Paola Pergami, Kristin P Guilliams, Melissa Chung, Ryan Felling, Michael M Dowling , Michael J Rivkin PMID: 31282248. PMCID: PMC9001020. DOI: 10.1177/0883073819855534 - N Engl J Med. 2014 Mar 20;370(12):1091-100. doi: 10.1056/NEJMoa1311367. Hemicraniectomy in older patients with extensive middle-cerebral-artery stroke Eric Jüttler 1, Andreas Unterberg, Johannes Woitzik, Julian Bösel, Hemasse Amiri, Oliver W Sakowitz, Matthias Gondan, Petra Schiller, Ronald Limprecht, Steffen Luntz, Hauke Schneider, Thomas Pinzer, Carsten Hobohm, Jürgen Meixensberger, Werner Hacke; DESTINY II Investigators
Collaborators, Affiliations Expand. PMID: 24645942. DOI: 10.1056/NEJMoa1311367 - Pediatr Neurol. 2018 Mar:80:70-76. doi: 10.1016/j.pediatrneurol.2017.11.015. Epub 2017 Dec 11. Hydrocephalus in Pediatric Traumatic Brain Injury: National Incidence, Risk Factors, and Outcomes in 124,444 Hospitalized Patients. Kavelin Rumalla , Vijay Letchuman , Kyle A Smith , Paul M Arnold
- Pediatr Neurol. 2018 Mar:80:70-76. doi: 10.1016/j.pediatrneurol.2017.11.015. Epub 2017 Dec 11. Hydrocephalus in Pediatric Traumatic Brain Injury: National Incidence, Risk Factors, and Outcomes in 124,444 Hospitalized Patients. Kavelin Rumalla , Vijay Letchuman, Kyle A Smith , Paul M Arnold .Affiliations Expand. PMID: 29429778 DOI: 10.1016/j.pediatrneurol.2017.11.015
About the Author

Rabia Qaiser
MD Indianapolis, USA
Rabia Qaiser, MD is an Associate Professor of neurosurgery and am dual fellowship trained in Pediatric (at Riley Children’s at Indiana University) and Cerebrovascular/Skull base neurosurgery (at Stanford University) with a passion for treating Pediatric Cerebrovascular diseases and Complex Tumors. She is also an associate program director. Outside of neurosurgery, She is a Cat-Mom to 3 – Zeppelin, Floyd, and Porchy – and like to read and photograph. She loves working with residents and fellows who teach her how to be a better mentor.
Graphics: Rabia Qaiser, MD
Medical Editors: Gayatra Mainali, MD
Junior Editor: Isabella Estrada