Background
This article builds on a previously published caregiver guide listed first in the Resources section, which introduces common therapy models for children with difficulties using one hand. Here, we extend that discussion to focus on how the quality of practice and amount of therapy interact—and why more therapy is not always better.
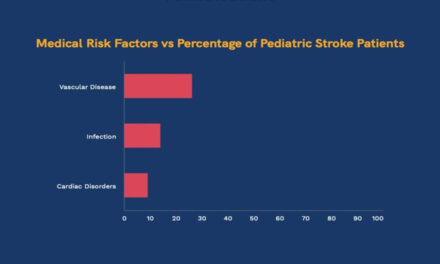
First, it’s helpful to understand how pediatric stroke relates to cerebral palsy (CP). CP is one of the most extensively studied childhood conditions in rehabilitation, providing a strong evidence base to guide therapy. Perinatal stroke (stroke occurring before, during, or shortly after birth) is the leading cause of CP affecting one side of the body (Kirton & DeVeber, 2013). When a stroke occurs later in childhood, it is referred to as a childhood stroke. After recovery has stabilized, the functional challenges following childhood stroke often look similar to CP, allowing us to confidently draw on CP research to guide therapy decisions after childhood stroke.
These are the key steps in evidence-based therapies for children with CP:
(1) Goal setting, where families and therapists together identify meaningful, motivating, time-limited goals.
(2) Implementation of a well-defined evidence-based therapy approach, which focuses on practicing these goals in therapy sessions and at home
(3) Evaluation, where progress towards goals is checked, development is reviewed, and next steps are planned.
Selecting the Therapy Model
As highlighted in the CP Traffic Light Review (Novak et al., 2020), different goals call for different therapy models. For example, strength training can improve muscle strength but doesn’t necessarily lead to better hand use or greater independence in daily activities. The Traffic Light Review and recent clinical practice guidelines (Jackman et al., 2022), recommend the following therapy models among the first line therapies for children with CP affecting one hand.
Skill-based therapy models
These include:
CIMT involves putting a glove, mitt, sling, or cast on the preferred hand and doing lots of practice with the hand they do not like to use. BMT encourages practice using toys and activities that involve both hands. These models help children develop and improve hand skills such as grasping, holding, and manipulating objects which are used during everyday activities like play, using utensils, or buttoning clothes. They are grounded in theories about how people best learn new skills, meaning your child needs to play an active role rather than being physically moved by the therapist. Children are encouraged to learn through problem-solving, feedback, practicing moderately challenging skills, and experiencing trial and error during fun and motivating activities (Greaves & Hoare, 2024). Activities must match your child’s goals.
Goal-Directed Training
Goal directed training (GDT) focuses on setting, practicing, and achieving meaningful goals. The aim is for your child to learn how to complete important activities efficiently and independently, like getting dressed, opening containers, or playing a game. There is no single “right” way to perform an activity because all humans perform tasks differently. Your child may perform some activities with one hand or adapt the way it is done compared to how we may do the task. While GDT is not aimed to improve hand skills, it is likely that your child’s hand skills will improve by repetitively practicing their motivating goal(s). As your child grows, GDT often becomes more important as they are expected to do more by themselves, need to get ready for school, and want more independence.
High-tech devices, splints, functional electrical stimulation (e-stim) and medical treatments such as injections of botulinum toxin-A (Botox) can be useful extras, but they should not replace first line therapies.
How much therapy is enough?
Therapy dosage refers to the total amount of time a child spends practicing with a therapist and with you at home. Across the different evidence-based therapy approaches, the ingredients, setting, and dose vary widely, making it difficult for families to determine how much therapy is needed. It is important for parents to first recognize that therapy can be scheduled in different ways. Intensive therapy approaches condense the total dose into daily sessions of high duration (e.g., 6 hours) over 2-3 weeks while distributed therapy approaches spread practice over a longer period (shorter daily sessions of about 30 minutes over 6 to 8 weeks. Research shows that both schedules are effective ways for implementing well designed, evidence-based therapy approaches (Liang et al., 2025; Wang et al., 2023; Sakzewski et al., 2015).
There is an assumption that more therapy is better and across the world there is a trend for families to seek very high-dose or “intensive” therapy programs (Taylor et al., 2025). However, research tells us that increasing the amount of therapy does not automatically lead to better outcomes (Hoare et al., 2013; Brandão et al., 2018; Ramey et al., 2021). It is important for parents to first recognize that therapy can be scheduled in different ways. Intensive therapy approaches condense the total dose into daily sessions of high duration (e.g., 6 hours) over 2-3 weeks while distributed therapy approaches spread practice over a longer period (shorter daily sessions of about 30 minutes over 6 to 8 weeks) (Paleg et al. 2025).
Although there is no single “right” number of hours, research offers general guidance. Jackman and colleagues (2020) suggest that skill-based therapies (such as BMT and CIMT) often show meaningful improvement after 30–40 hours of practice, while GDT requires 14–25 hours of practice per goal. These figures should be viewed as general guidance as the amount of practice is not simply guided by the name of a therapy model. It is one part, or one important ingredient of a specific therapy approach along with all the other important strategies that make the approach effective (Taghizadeh et al., 2025). Once a therapy approach has been selected based on your child’s goals, your therapist should support you in understanding the right amount of practice.
High-quality therapy helps children think, try, adjust, and problem-solve using strategies grounded in how people best learn skills and generalize them to their daily lives. You should see your child thinking and doing during therapy sessions (Hoare & Greaves, 2017). They should be practicing their specific goals. Without these elements, even large amounts of practice may have limited benefit. In addition, excessive hand-over-hand assistance (therapist moves the child’s hands), passive weight bearing through the hands (without practicing hand skills for daily tasks), reflex-based movements (triggered by the therapist rather than the child), or positioning unrelated to your child’s goals are unlikely to support meaningful learning or goal achievement.
Regardless of the dosage, research shows us that children vary widely in how they respond. Some make large gains during a single block of therapy, while others show smaller or slower changes (Hilderley et al., 2025; Sakzewski et al., 2025; Taylor et al., 2025). Children who respond especially well are often highlighted on social media, which can unintentionally create unrealistic expectations for families. Research also suggests that some children who do not make large gains from one block of therapy may benefit from multiple blocks over time (Taylor et al., 2025). Therefore, it is important that therapy for your child is viewed as a long-term journey throughout childhood, rather than a one-time event.
Timing Matters—but Learning Continues Across Childhood
This pattern reflects how skills are acquired and refined over time, rather than a point at which learning stops. Importantly, slower rates of change at older ages do not mean therapy is ineffective. Children who begin therapy later, or who continue therapy beyond the early years, can still improve function and learn new skills when therapy emphasizes active, goal-directed practice.
Take-home message: you don’t need to travel far or spend more money chasing the most intensive program for your child. Ask your child’s therapist about evidence-based therapy options that fit your child’s goals and motivation—whether delivered through weekly sessions with a home program or a short intensive block—knowing that the most effective approaches are also the most accessible and flexible, built on meaningful collaboration between the child, family, and therapist.
Disclaimer The first author serves as Co-Editor-in-Chief of Kid Stroke Connection, the official publication of the International Pediatric Stroke Organization. This article reflects the author’s independent clinical and research experience and does not imply editorial endorsement.
Resources
1. Information Education Page, Archives of Physical Medicine and Rehabilitation (2023)
2. Cerebral Palsy Foundation (2020)
Considering alternatives: A guide to decision-making for cerebral palsy treatments. https://cpresource.org/topic/treatment-options/considering-alternatives-guide-decision-making-cerebral-palsy-treatments
3. Todd J. Levy, MS, OTR/L, CBIST-AP
- Children’s Hospital of Philadelphia
4. Brian Hoare, B.O.T; PhD
- Cerebral Palsy Group, 74 Faraday Street, Carlton, Victoria 3053 Australia
- 2 – School of Allied Health, Australian Catholic University, 115 Victoria Parade, Fitzroy, VIC 3065, Australia
- 3 – Discipline of Occupational Therapy, La Trobe University, Plenty Road, Bundoora, VIC 3086, Australia
References
- de Brito Brandão, M., Mancini, M. C., Vaz, D. V., Pereira de Melo, A. P., & Fonseca, S. T. (2010). Adapted version of constraint-induced movement therapy promotes functioning in children with cerebral palsy: a randomized controlled trial. Clinical rehabilitation, 24(7), 639-647.
- Cerebral Palsy Foundation. (2020). Considering alternatives: A guide to decision-making for cerebral palsy treatments. https://cpresource.org/topic/treatment-options/considering-alternatives-guide-decision-making-cerebral-palsy-treatments
- Greaves, S., & Hoare, B. (2024). Upper Limb Therapy for Infants and Young Children with Unilateral Cerebral Palsy: A Clinical Framework. Journal of Clinical Medicine, 13(22), 6873.
- Jackman ML, Sakzewski L, Morgan C, et al. Clinical practice guideline for the use of upper limb therapies in children with unilateral cerebral palsy. Dev Med Child Neurol. 2022;64(5):536–549. https://doi.org/10.1111/dmcn.15162
- Novak I, Morgan C, Adde L, et al. Early, evidence-based intervention for cerebral palsy: the updated “Traffic Light” systematic review. Dev Med Child Neurol. 2020;62(1):85–90. https://doi.org/10.1111/dmcn.14446
- Levy TJ, Hoare BJ. Therapy choices for children with difficulties using one hand after a brain injury. Arch Phys Med Rehabil. 2023;104(11):2315–2322.
- Kirton A, DeVeber G. Life after perinatal stroke. Stroke. 2013;44(11):3265–3271.
- Jackman M, Sakzewski L, Morgan C, et al. Upper limb practice dosing for children with unilateral cerebral palsy: a systematic review. Dev Med Child Neurol. 2020;62(4):498–505.
- Hilderley AJ, Dunbar M, Andersen J, et al. Neuromodulation for Children With Hemiparesis and Perinatal Stroke: A Randomized Clinical Trial. JAMA Neurol. 2025;82(3):267–275.
- Hoare, B., & Greaves, S. (2017). Unimanual versus bimanual therapy in children with unilateral cerebral palsy: Same, same, but different. Journal of Pediatric Rehabilitation Medicine, 10(1), 47-59.
- Hoare BJ, Imms C, Villanueva E, Rawicki HB, Matyas T, Carey L. Intensive therapy following upper limb botulinum toxin A injection in young children with unilateral cerebral palsy: a randomized trial. Dev Med Child Neurol. 2013;55(3):238–247.
- Hoare BJ, Wallen MA, Imms C, Villanueva E, Rawicki HB, Carey L. Constraint-induced movement therapy in children with unilateral cerebral palsy. Cochrane Database Syst Rev. 2019;4(4):CD004149.
- Gordon AM, Schneider JA, Chinnan A, Charles JR. Efficacy of a hand–arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: a randomized control trial. Dev Med Child Neurol. 2007;49(11):830–838.
- Nordstrand, L., Eliasson, A. C., & Holmefur, M. (2016). Longitudinal development of hand function in children with unilateral spastic cerebral palsy aged 18 months to 12 years. Developmental Medicine & Child Neurology, 58(10), 1042-1048.
- Paleg, G., Pool, D., Hidalgo-Robles, Á., Frumberg, D., Livingstone, R., & Damiano, D. (2025). Where’s the Evidence? Challenging Therapists to Stop Legitimizing Dynamic Movement Intervention and Cuevas Medek Exercises. Pediatric Physical Therapy, 10-1097.
- Ramey, S. L., DeLuca, S. C., Stevenson, R. D., Conaway, M., Darragh, A. R., & Lo, W. (2021). Constraint-induced movement therapy for cerebral palsy: A randomized trial. Pediatrics, 148(5).
- Sakzewski, L., Greaves, S., Eliasson, A., Wallen, M., Novak, I., Ware, R. S., … Sakzewski, L., Greaves, S., Eliasson, A. C., Wallen, M., Novak, I., Ware, R. S., … & Boyd, R. N. (2025). Early developmental trajectories of the impaired hand in infants with unilateral cerebral palsy. Developmental Medicine & Child Neurology, 67(7), 901-909.
- Sakzewski, L., Miller, L., Ziviani, J., Abbott, D. F., Rose, S., Macdonell, R. A., & Boyd, R. N. (2015). Randomized comparison trial of density and context of upper limb intensive group versus individualized occupational therapy for children with unilateral cerebral palsy. Developmental Medicine & Child Neurology, 57(6), 539-547.
- Taylor, E., Greaves, S., & Hoare, B. (2025). Barriers, Facilitators, and a Proposed Model of Care for Implementation of Upper Limb Distributed Practice Approaches for Children with Unilateral Cerebral Palsy. Journal of Clinical Medicine, 14(3), 924.
- Taghizadeh, A., Webster, K. E., Bhopti, A., Carey, L., & Hoare, B. (2023). Are they really motor learning therapies? A scoping review of evidence-based, task-focused models of upper limb therapy for children with unilateral cerebral palsy. Disability and Rehabilitation, 45(9), 1536-1548.
- Wang, T. N., Perlmutter, M. S., Muzzio, S. L., Eliasson, A.-C., Gordon, A. M., & Coker-Bolt, P. (2023). Effects of intensive versus distributed constraint-induced movement therapy for children with unilateral spastic cerebral palsy: A multisite randomized controlled trial. Physical & Occupational Therapy in Pediatrics, 43(6), 623–637.
About the Author

Todd J. Levy, MS, OTR/L, CBIST-AP
Todd Levy, MS, OTR/L, CBIST, is a clinical specialist at The Children’s Hospital of Philadelphia where his efforts include direct clinical care, clinical quality improvement, research investigation, program development and training. Mr. Levy’s interests include pediatric stroke and traumatic brain injury, hand therapy, vestibular therapy, and improving patient-caregiver engagement in the healthcare process using technology.
Mr. Levy has worked with children with brain injuries and their caregivers from acute care, to inpatient rehabilitation, to outpatient and school settings. He began his career at Washington University in St. Louis studying the effects of neonatal hypoxic ischemic brain injury, neuroprotective agents and environmental enrichment on neurodevelopmental outcomes. Mr. Levy has been involved in brain injury education and prevention endeavors through the Brain Injury Association of America. He serves on the Board of Governors of the Academy of Certified Brain Injury Specialists.
Medical Editors: Gayatra Mainali
Junior Editor: Christine Zhang